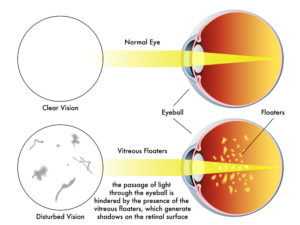
In order to properly examine your retina, a dilated eye exam is necessary each and every time you come to the office. A dilated eye exam requires use of dilating drops to dilate and enlarge your pupils to allow us to properly diagnose and treat diseases of the retina.
A dilated eye exam is the only way the retina can be examined by direct visualization using a combination of lenses and specialized ophthalmic instruments.
Other methods such as photography, fluorescein angiography, optical coherence tomography (OCT) and ultrasound can be used in conjunction to direct visualization to diagnose and to treat retinal diseases.
As a retina specialist, virtually everyone of my patients needs a dilated eye exam every time they come to the office.
Dilating Eye Drops
There are several drops used routinely to dilate the eyes. All are marked with a bright red cap to distinguish these eye drops from other types.
In most cases, we only need to use phenylephrine and tropicamide do satisfactorily dilate the pupils. These drops work differently to achieve dilation.
Tropicamide inhibits the small muscle located at the margin of the pupil. The function of the pupillary sphincter muscle is to constrict the iris in bright light and makes the pupil smaller through a purse-string mechanism. Tropicamide prevents this constriction.
Phenylephrine stimulates another set of muscles which function to enlarge the pupil. The iris dilator muscle runs radially along the iris and, when stimulated, pulls the iris open.
Cyclopentolate and atropine can also dilate the pupils but their effects last much longer (days to weeks) and are generally not used for diagnostic purposes.
How Long does Dilation Last?
In most circumstances, your eyes will stay dilated for several hours after the exam. Several factors influence the length of time your eyes will stay dilated, such as:
- Color of your eyes
- Your age
- Type, strength and amount of the medicine
- Previous eye surgery
Lightly colored eyes, such as blue and hazel, dilate very quickly and stay dilated longer compared to brown eyes.
Brown eyes actually contain brown colored pigment which absorbs the dilating medicine, whereas blue eyes actually contain no pigment and the eyes dilate faster.
Younger eyes tend to take a longer time to dilate. Certain diseases (e.g. iritis) can make dilation take a very long time.
Dilation usually takes at least 20 minutes at a minimum and will reverse after a few hours.
If you would like to schedule an appointment, please call us (877) 245.2020.