Hydroxychloroquine has long been used to safely treat patients with malaria and certain autoimmune diseases such as lupus erythematosus and rheumatoid arthritis, but NOT COVID019.
In the news, there have been small, inconclusive studies using two malaria and autoimmune medications to treat COVID-19 (coronavirus 2019). Some studies suggest the medications might be helpful, while other studies saw no difference.
Currently, there is not enough medical data to prove that hydroxychloroquine and chloroquine work for COVID-19.
Hydroxychloroquine Approved for Malaria
Chloroquine was approved by the FDA in 1949 as a treatment for malaria, an infection caused by a parasite. Hydroxychloroquine was approved by the FDA in 1955 for the treatment of malaria. Hydroxychloroquine is preferred over chloroquine because it has fewer side effects.
Both drugs are available in pill form. Plaquenil is also approved for long-term use in rheumatoid arthritis and lupus.
The side effects of both medications include:
- Retinal damage and irreversible vision loss (Plaquenil Toxicity)
- Headache
- Abnormal heart rhythm
- Muscle weakness or nerve pain
- Gastrointestinal issues (nausea, cramping, vomiting, and diarrhea)
- Hypoglycemia (low blood glucose)
- Worsening of psoriasis
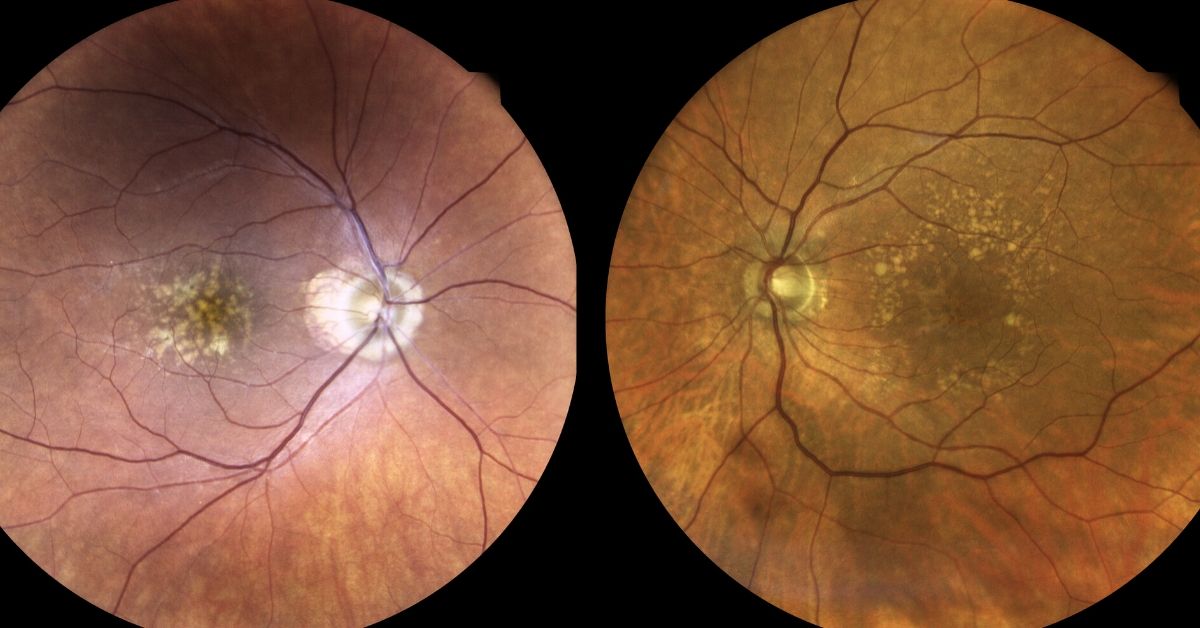
Retinal Damage | Plaquenil Toxicity
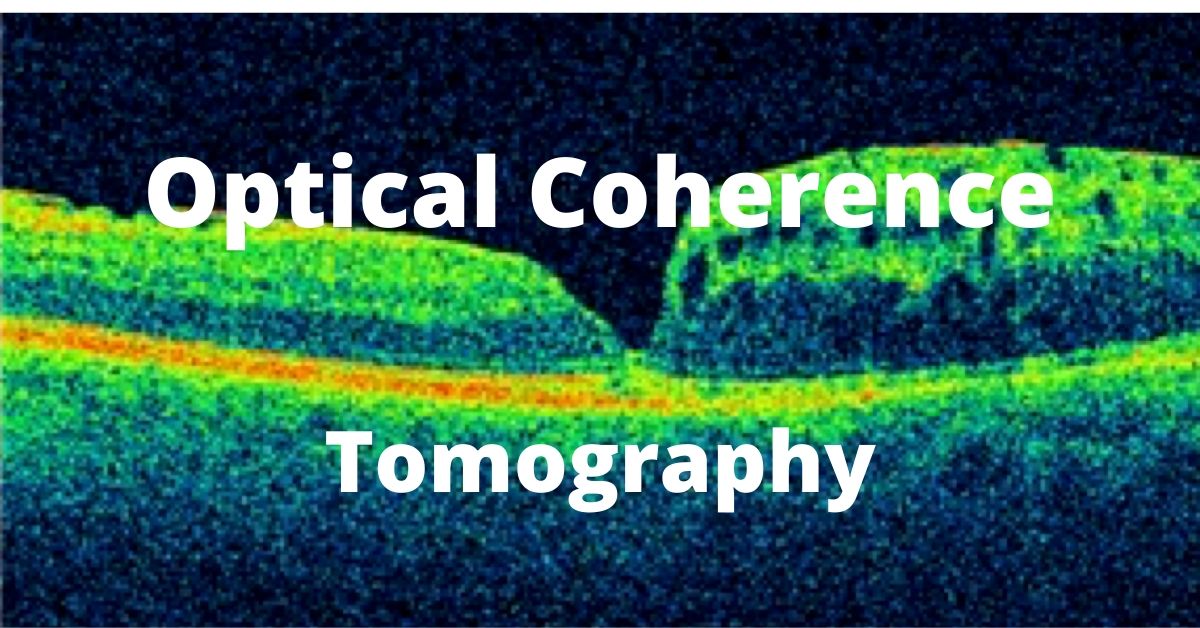
The overall prevalence of chloroquine/hydroxychloroquine retinopathy is 7.5%. Retinal damage is one of the most serious adverse effects of hydroxychloroquine (HCQ) since the retinal damage caused by the drug is irreversible. Chloroquine/hydroxychloroquine retinopathy is more common with higher daily doses and long-term use.
A baseline retinal examination is recommended for all patients taking HCQ, along with regular monitoring examinations. The baseline and monitoring examinations should include the following:
- Uncorrected visual acuity test
- Best-corrected visual acuity test
- Examination with ophthalmoscope
- Examination using slit-lamp
- Optical Coherence Tomography
The FDA previously issued an Emergency Use Authorization (EUA) that allows physicians to request a supply of hydroxychloroquine or chloroquine for hospitalized patients with COVID-19 who are unable to join a clinical trial.
As of this writing 4/24/20, the FDA now warns against the use of hydroxychloroquine for the treatment of COVID-19 after reports of irregular heart rhythms and deaths.
If you are presently taking Plaquenil, talk to your prescribing doctor to insure that you are getting regular eye exams.
If you would like to schedule an appointment, please call us (877) 245.2020.