As the COVID-19 pandemic continues to spread, the American Academy of Ophthalmology (AAO), the Centers for Disease Control and Prevention (CDC) and the American Hospital Association have issued recommendations aimed at reducing exposure and preserving healthcare resources, aka, “flattening the curve.”
Will this affect all eye doctors? Will this affect you?
Stop Routine Care
The American Academy of Ophthalmology is recommending that eye doctors stop routine eye care at this time and focus only on those patients with urgent and emergent conditions. Examples of “routine” care might include glasses prescriptions, routine follow-up or cataract evaluations.
Please check with your own doctor if you need to be seen.
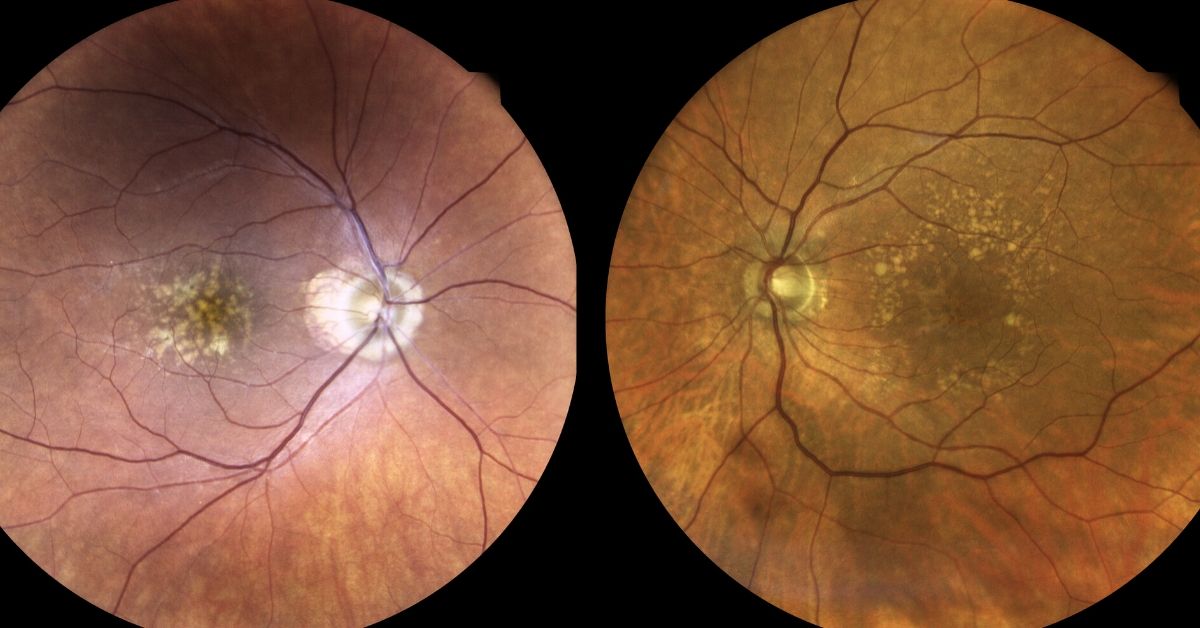
As a retina specialist, I may not necessarily “need” to see a patient I see every 6 months with diabetes who is not noticing any changes since the last visit, but I may need to evaluate someone who recently lost vision or developed pain.
By limiting the number of patients who come through our offices, we are protecting our patients, our staff and ourselves from exposure to the virus. It is our way of increasing the likelihood that a patient may remain in place and limit the spread of this disease.
Stop Elective Surgery
Both the American Hospital Association and the Centers for Disease Control and Prevention are recommending that hospitals stop performing elective surgery and non-urgent surgical procedures. Examples of each might include joint replacements and cataract surgery. Non-urgent surgical procedures might include a colonoscopy.
What’s the rationale? It saves resources.
Elective surgeries and procedures take up hospital resources. By canceling or postponing these procedures, for example, hospital beds and staff can be freed to help with more critical patients elsewhere in the hospital system.
Nurses and aides who normally work in an elective surgical center may be needed elsewhere such as the emergency room.
This practice will also limit exposure to healthy patients.
Don’t forget that while this pandemic is progressing, patients will still need emergency surgery, chemotherapy, and require care for heart attacks and strokes.
This is an effort to avoid overburdening our hospital resources and “flatten the curve.”
If you would like to schedule an appointment, please call us (877) 245.2020.