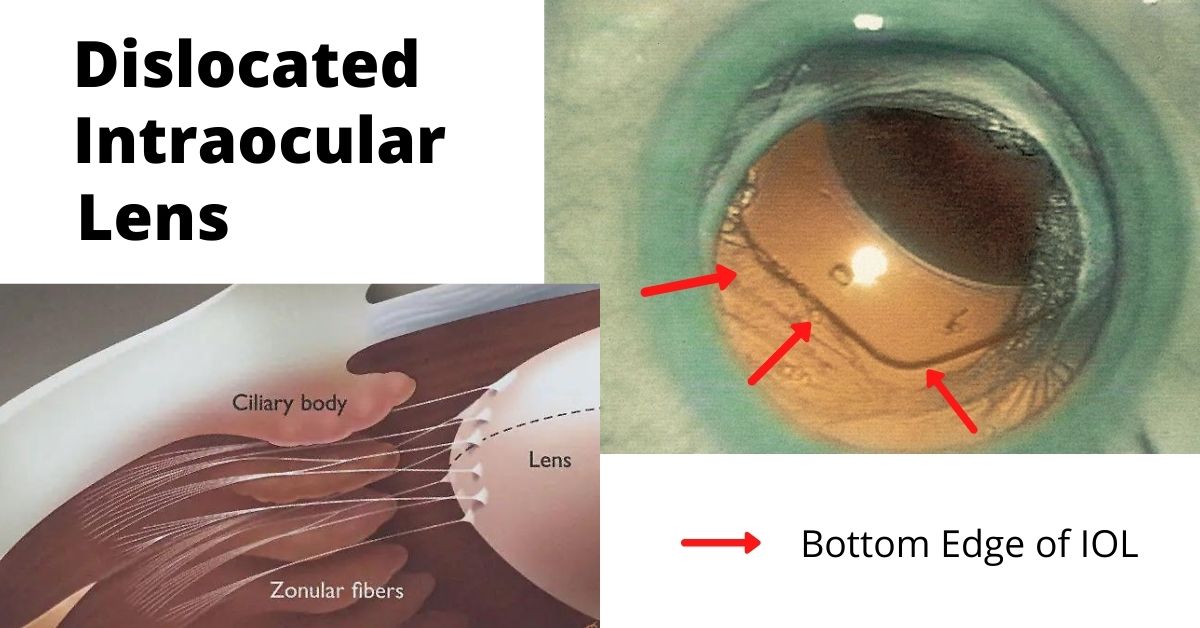
A dislocated intraocular lens is very similar to a dislocated crystalline (natural) lens. The only difference is that the intraocular lens has been inserted during previous cataract surgery.
Cataract surgery is a low-risk surgery and has a success rate of about 95%. But like all surgeries there can be complications, especially if you have other eye or health issues.
One of those complications is a dislocated intraocular lens (IOL). This is a rare complication and occurs in less than 3% of cases, but it may require additional surgery to repair.
What causes a Dislocated?
Sometimes the dislocation happens shortly after cataract surgery because the zonules, a ring of tiny thread-like fibers that support and hold the lens capsule in place, fail or break. The zonules are made of a connective tissue protein. People who have a connective tissue disorder are more likely to have this complication, and it can also occur in patients who have a history of previous eye surgeries, trauma to the eye, or who take prostate medication.
Other times the IOL dislocation happens gradually over time when the zonules slowly weaken and don’t adequately support the lens capsule and this causes the lens to shift away from the center of the pupil. This happens more often in patients with a history of eye trauma, multiple eye surgeries, especially retinal detachment repair, and complicated original cataract surgery.
Symptoms
The most common symptom of a dislocated IOL is blurry vision. The degree of blurriness depends on how dislocated the IOL is. If the IOL is only slightly dislocated then vision may still be clear, but ghost images or a double image at night may occur when light passes through the edge of the dislocated lens.
Treatments
Treatment depends on the severity of the dislocation. Some dislocations very minor and vision is still good. In these cases, no treatment is necessary.
If the lens is completely off center and vision is very blurry, then only surgery will correct it. In some cases, the original implanted IOL can be repositioned and secured in place. In other cases when the zonules are extremely weak or damaged, a new IOL designed to be sutured to the wall of the eye (sclera) or to the iris is used.
If the lens has fallen into the vitreous cavity, then a retinal surgeon will need to perform a vitrectomy to remove the vitreous jelly inside the eye and retrieve the dislocated intraocular lens.
Prognosis
Most patients who have IOL repositioning or IOL replacement have vision of 20/40 or better after surgery. The outcome depends on your health and if you have other eye issues, such as macular degeneration or diabetic retinopathy.
Recovery for IOL replacement is similar to the recovery time for cataract surgery. The medications are the same and most patients can resume normal activities the day after surgery.
If you would like to schedule an appointment, please call us (877) 245.2020.