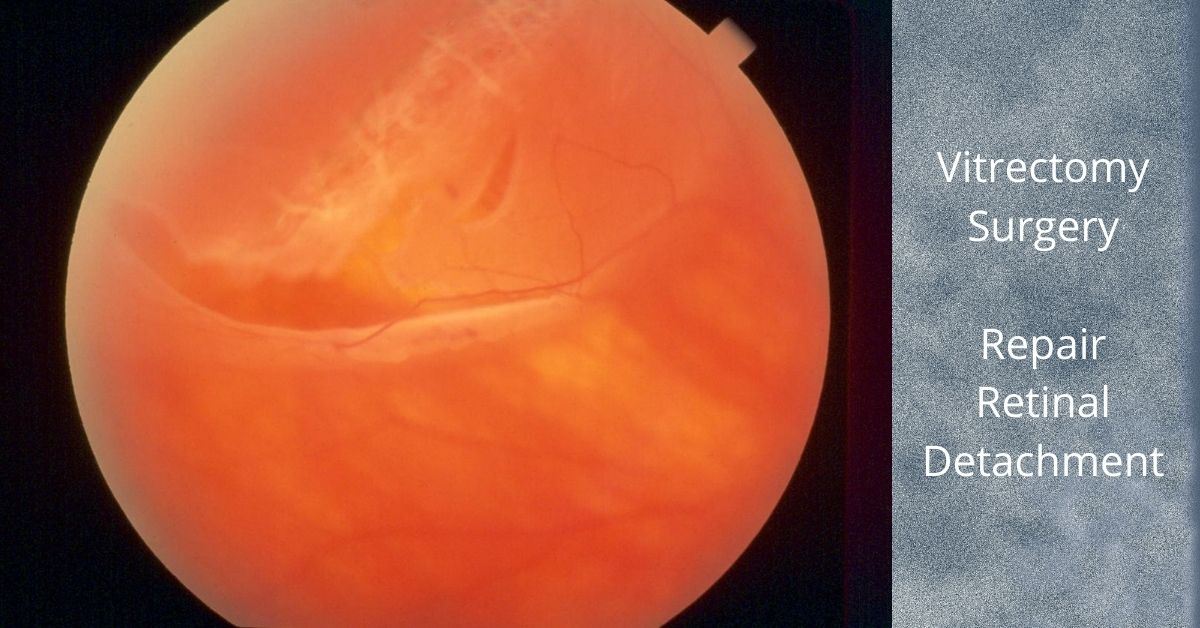
Vitrectomy for retinal detachment repair is an alternative method to scleral buckle or pneumatic retinopexy.
A vitrectomy is a common surgical repair for a detached retina. The surgery removes the vitreous gel from the eye, pushes the detached retina back into place, and seals any retinal tears in the retina. Then gas is injected into the eye to help keep the retina in place and prevent any fluid from leaking from the repaired tears and into the subretinal space.
The Surgery
A vitrectomy is usually performed using local anesthetic. A heavy sedative is administered and then Lidocaine is injected around the eye to numb it. If patients prefer not to be awake during the procedure they can be given intravenous sedation or a general anesthesia.
The surgery consists of making three small needle-sized incisions (about the width of an eyelash) into the white part of the eye (sclera). Through one incision a constant flow of fluid is passed into the eye. The second incision is used to insert a fiber-optic light to provide illumination of the eye, and the third is for any instruments that are used, including a “vitrector” for the removal of the vitreous.
A vitrector is an oscillating microscopic cutter that slowly removes the vitreous. Once the vitreous is removed, a freezing instrument or a laser is used to seal any tears in the retina.
The vitreous will be replaced with a gas. In time the gas will dissipate and be replaced by the eye’s own fluids (aqueous humor). The vitreous gel does not grow back, but the eye can function with just the fluid that replaces the vitreous. Depending on the type of gas used and its concentration, it can take from three to ten weeks to fully dissipate.
Most retina specialists will perform vitrectomy for retinal detachment repair in an outpatient setting. The surgery time ranges from 20 to 40 minutes, but varies greatly.
Head positioning
Head positioning after surgery is necessary to keep the gas bubble in the proper place. If the retina detached at the bottom, the only way to get the bubble to press against the place of detachment is to place the head down. The bubble walls off the damaged area while it heals and prevents any fluid from flowing through the damaged area of the retina and into the subretinal space.
The gas bubble wiur vision while it is in place, but as it dissipates a line will form across your vision where the newly forming fluid (aqueous humor) is gradually replacing the bubble. The line will move lower each day and the field of vision will get larger.
If you have to position your head down there are pillows, chairs, and mirrors that allow you to see around the room while in a face-down position.
Gas bubble precautions
As long as the gas bubble remains in your eye, you must not fly in an aircraft. The reduced pressure in the cabin will cause the gas bubble to expand. This would be extremely painful and could lead to loss of sight. If you must have general anesthesia for any surgical procedure while the gas bubble is in your eye, you must inform your anesthesiologist so you will not be given nitrous oxide, which would cause a dangerous rise in eye pressure in the eye with the gas bubble.
Safety
Vitrectomy surgery was first developed in 1970 and since then many improvements in instrumentation and technique have dramatically improved the safety of the procedure. Severe complications are rare and the surgical success rate is over 90%.
Nader Moinfar, M.D., M.P.H.
Retina Specialist
Orlando, FL
If you would like to schedule an appointment, please call us (877) 245.2020.