The retina is a highly specialized layer of tissue that lines the inside of the eye. As part of the central nervous system, it serves as a crucial component of the visual system. Its primary function is to convert light into electrical signals that can be translated to “vision” by our brain.
It consists of several layers of cells, each with a specific role in the process of vision. The outermost layer contains the photoreceptor cells, known as rods and cones. Rods are responsible for vision in low-light conditions and are highly sensitive to light, while cones are responsible for color vision and visual acuity in brighter light conditions. Cones are further classified into three types: red, green, and blue cones, allowing us to perceive a wide range of colors.
Converts Light to Electrical Signals
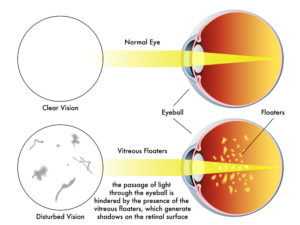
When light enters the eye, it passes through the cornea and lens, which help focus the light onto the retina. The rods and cones in the retina absorb the light and convert it into electrical signals. This process involves the activation of light-sensitive pigments within the photoreceptor cells, triggering a cascade of chemical reactions that generate electrical signals.
The electrical signals produced by the rods and cones are then processed by several layers of cells within the retina. Bipolar cells receive the signals from the photoreceptor cells and transmit them to ganglion cells, which are the final layer of cells in the retina. The ganglion cells collect the signals and their axons form the optic nerve, which carries the visual information from the retina to the brain.
Highly Specialized Cells Sharpen Vision
Within the retina, there are also other types of cells, such as horizontal cells and amacrine cells, which help refine and modulate the visual signals. These cells play a role in enhancing contrast, adjusting sensitivity to light, and facilitating communication between different parts of the retina.
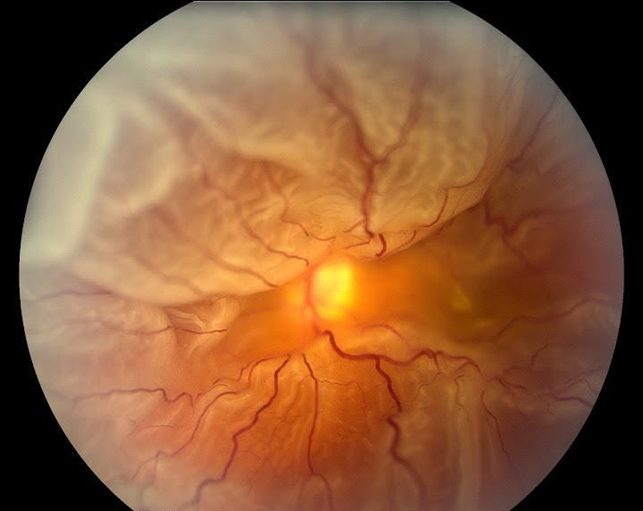
The central region of the retina is known as the macula, which contains a high concentration of cones. At the center of the macula is a small depression called the fovea, where visual acuity is highest. The fovea contains a high density of cones, allowing for detailed and sharp central vision.
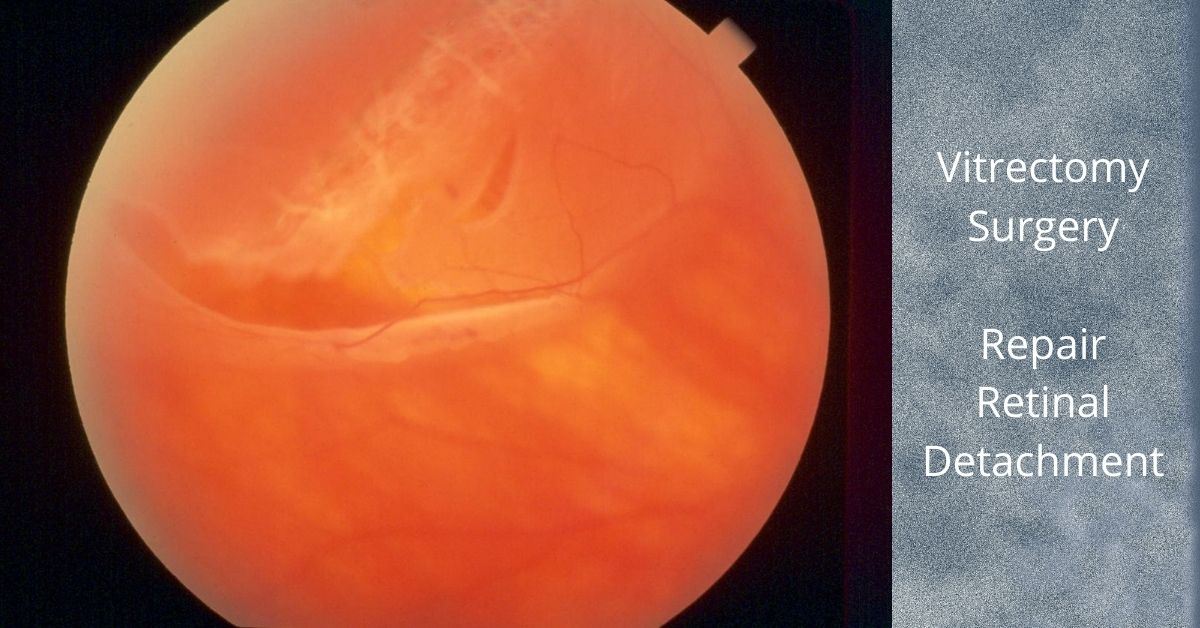
For us to see, all layers of the retina must be healthy, maintain normal blood supply and remain attached.
If you would like to schedule an appointment, please call us (877) 245.2020.