A retina specialist is an ophthalmologist who has extra-training in diseases and surgery of the retina. Additional training years are required to focus attention in this special area.
Here are 7 more common reasons why you may be referred to a retina specialist.
Retinal Tear, Retinal Detachment, Retina Specialist
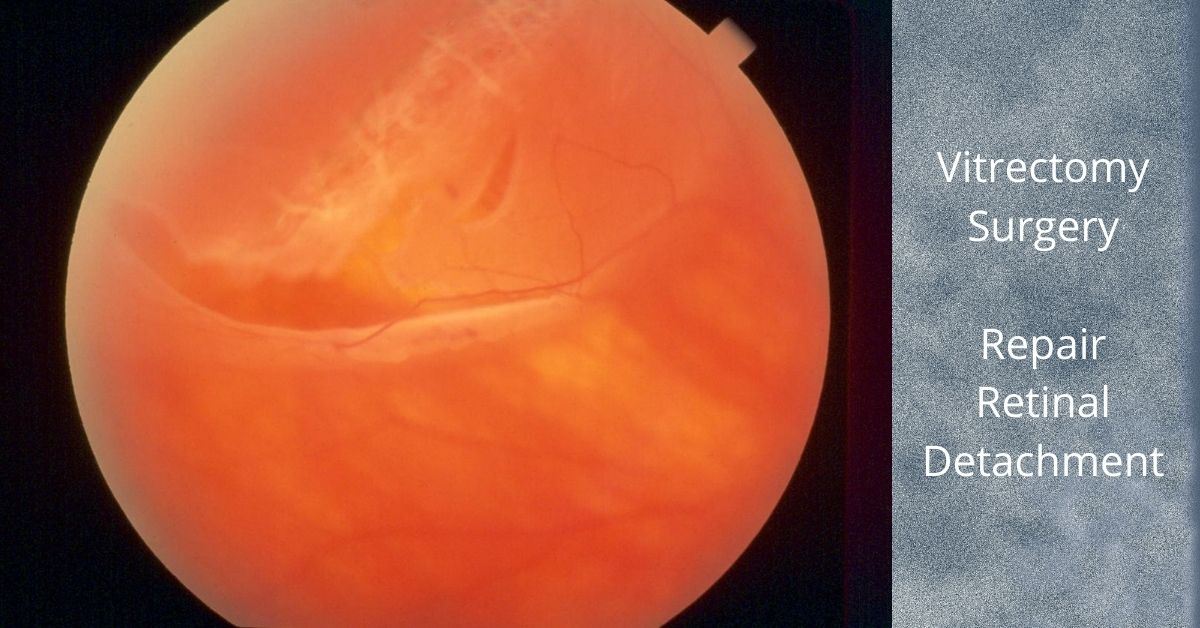
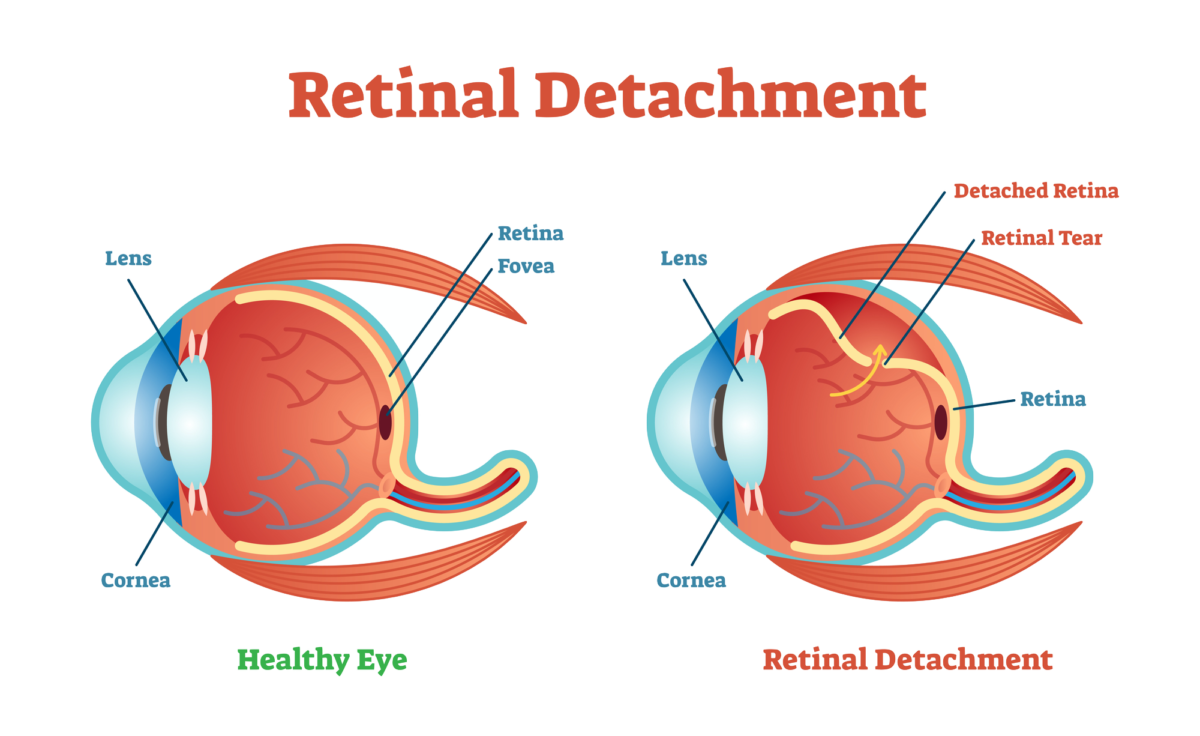
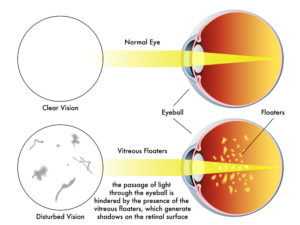
Retinal tears can cause a retinal detachment. Retinal tears may be asymptomatic, but often are associated with the sudden onset of new floaters or flashes usually due to a posterior vitreous detachment.
While most new floaters and flashes are NOT associated with a retinal tear, the only way to make sure you are not at risk for developing a retinal detachment is have a complete dilated eye exam.
Retinal tears can be treated with either cryotherapy or laser. Retinal detachments will often require surgery.
Foreign Body Inside the Eye
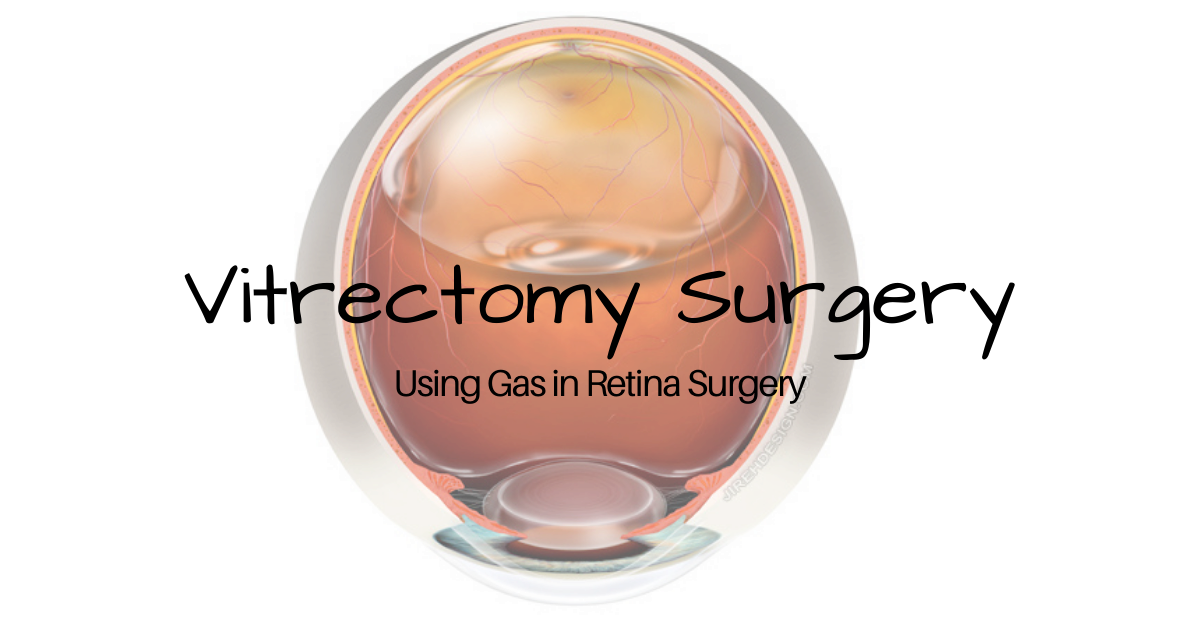
While not commonplace, intraocular foreign bodies may occur with any penetrating eye injury. Glass, metals and organic material need to be removed by performing a vitrectomy, the principal operation performed by a retina specialist.
Retina Specialist and Endophthalmitis
Endophthalmitis is infection inside the eye. This usually occurs following recent eye surgery, but can also follow penetrating eye injury.
Prompt referral to a retina specialist is paramount in preventing loss of vision from infection. Intraocular antibiotics, anti-fungals and/or vitrectomy surgery may be necessary to prevent catastrophic vision loss.
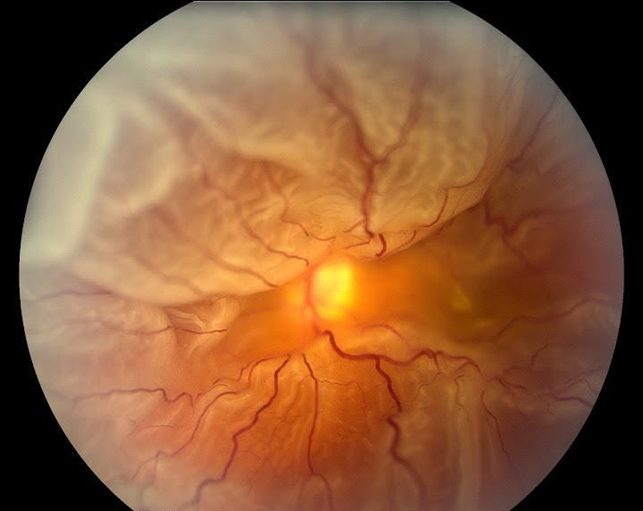
Advanced Diabetic Retinopathy
Diabetic retinopathy can cause blurry vision and blindness. A retina specialist is adept at treating the two most common causes of vision loss from diabetes: diabetic macular edema and proliferative diabetic retinopathy.
Common treatments used by retina specialists include: anti-VEFG injections, steroids, laser and surgery. In most scenarios, these are procedures only offered by a retina specialist.
Macular Degeneration
Macular degeneration (AMD) comes in two forms: dry AMD and wet AMD. The “wet” form is also called neovascular AMD (nAMD).
Both types of macular degeneration affect both eyes and are progressive, but the wet form can steal vision quickly, is associated with leaky abnormal blood vessels and bleeding. Treatment usually involves intravitreal injections of anit-VEGF.
There is presently no treatment for dry macular degeneration approved by the FDA.
Retinal Vascular Occlusions
Periodically the retinal vessels can become occluded or blocked. Both arteries and veins can be blocked retinal vascular occlusions. Vision loss is usually sudden and treatments may be required in an attempt to improve vision and/or to prevent total blindness from complications of the vascular occlusions.
If you would like to schedule an appointment, please call us (877) 245.2020.