Retina surgery is complex and requires exacting precision within the microscopic space of the retina. Recent advances in the size and precision of surgical instruments, microscopic viewing systems, and vitrectomy machines with multiple customizable controls have enabled retina repairs that were impossible just a decade ago.
In addition, these advances in technology have reduced operating times and many retinal repairs take less than an hour and can be done under a local anesthetic and a mild sedative at an outpatient surgical site.
Retina Surgery
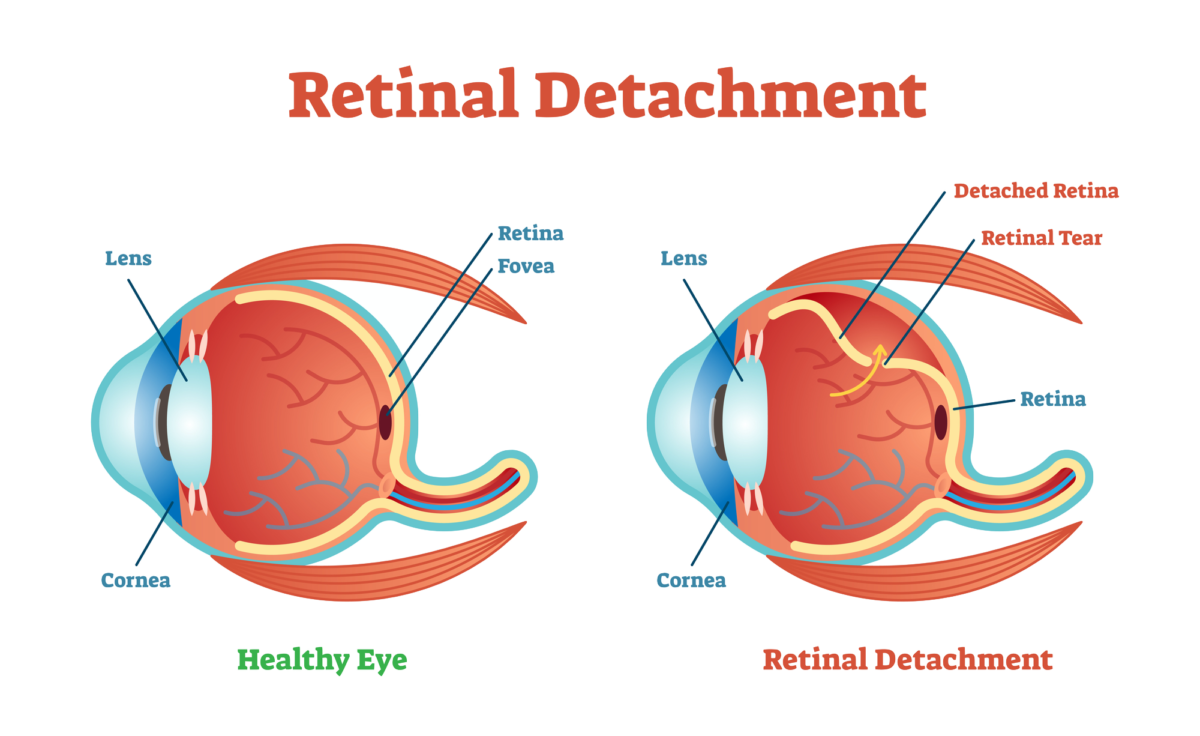
To repair retinal holes or tears, remove scar tissue, or reattach a detached retina, the retina specialist must have access to the retina. To do that the vitreous humor gel that fills the eye cavity is removed in a procedure called a vitrectomy. Once the vitreous humor gel is out of the way, the surgeon makes the needed repairs to the retina.
An EKG and blood pressure, and oxygen sensors are placed to monitor vital signs and sedation is administered through an IV. The sedation puts you in a twilight state in which you are very sleepy and relaxed yet still able to hear your surgeon and respond to simple instructions.
Eye drops are used to numb the eye. Once the eye is numb an eyelid holder is placed to prevent blinking during the surgical procedure. The eyelid holder is not uncomfortable because while your eyes are numb you will not have the sensation of needing to blink.
The Gas Bubble
After your retina is repaired a gas or air bubble is used as a tamponade to prevent the fluid that naturally exudes from inflamed tissues from reaching your retina. The gas bubble walls off and protects the repaired retina while it heals. The gas bubble gradually dissipates and is replaced by natural aqueous fluid.
There are two medical gases that are commonly used. One of them dissipates in 10 to 14 days, whereas the other takes 55 to 65 days to dissipate. If air is used as the bubble, it will absorb within 5 to 7 days.
Depending on your repair, your retina specialist will choose the appropriate medical gas with the correct absorption time.
The gas bubble makes vision extremely out of focus while it covers the entire vitreous chamber. While it dissipates a line will appear in your vision where the bubble is gradually being replaced by aqueous humor. The line will move further down, and your field of vision will grow larger day by day.
You will be instructed not to fly in an airplane as long as any of the gas bubble remains in your eye. The bubble can expand in the reduced pressure of an airplane cabin causing severe pain and possible loss of sight.
Head Position
You may be asked to keep you head face down during your recovery to keep the gas bubble in the correct position. You can get face down pillows, chairs, and mirrors to help you see things around you while your head is face down. Your insurance might cover the cost of some of the face down recovery equipment.
After Your Retina Surgery
Your eye will be patched after surgery and you will be asked to wear the patch for a day or two following surgery. Recovery time depends on the procedure you had, but ranges from two weeks to several months for a repaired detached retina.
If you would like to schedule an appointment, please call us (877) 245.2020.